State lawmakers are considering a bill meant to protect access to HIV prevention drugs for insured Californians as threats from the federal government continue.
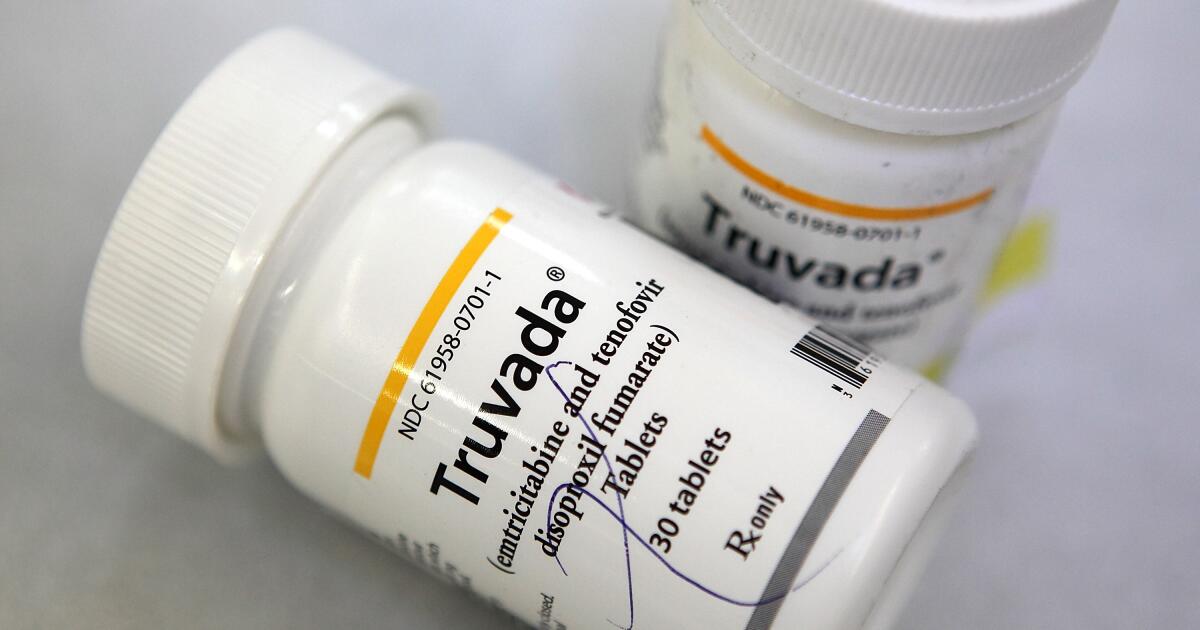
Assembly Bill 554 would require health plans and insurers to cover all antiretroviral drugs used for PrEP and PEP regimens. The drugs just have to be approved by the Food and Drug Administration, and would not require prior authorization. The bill would also prevent health plans from forcing patients to first try a less expensive drug before choosing a more expensive, specialty option.
The bill requires insurance providers to cover these drugs without cost-sharing with patients, and it limits the ability of insurers and employers to review treatments to determine medical necessity. To streamline reimbursements and expand the range of PrEP medications doctors can pick for their patients, the legislation allows providers to directly bill insured patients’ pharmaceutical benefit plans.
LGBTQ+ public health advocates worry that the Trump administration’s recent attempt to slash $1.5 billion in HIV prevention funding from the federal budget — along with its decisions to stop offering suicide-prevention counseling for LGBTQ+ individuals through the national 988 lifeline and to restrict gender-affirming care for transgender Americans — amounts to an assault on the queer community.
The state bill would act “as a shield against this administration’s cruelty,” said California Assemblymember Mark González (D-Los Angeles) who co-sponsored AB 554 with Assemblymember Matt Haney (D-San Francisco).
A recent cause for alarm among LGBTQ+ health advocates, first reported in the Wall Street Journal, is news that Health and Human Services Secretary Robert F. Kennedy Jr. plans to replace the entire U.S. Preventive Services Task Force because its 16 appointed members are too “woke,” according to unnamed individuals cited by the Journal.
At a news conference Monday, Kennedy confirmed that he is reviewing the makeup of the panel, adding that he hasn’t made a final decision.
The bill was introduced earlier in the year out of fear that Kennedy’s skepticism about vaccines might spill over into HIV/PrEP drug coverage and because of worries that President Trump would dismantle the task force, González said.
The task force wields immense influence, making recommendations about which cancer screenings, tests for chronic diseases and preventive medications are beneficial for Americans and therefore should be covered by insurers — including drugs for HIV/AIDS prevention.
Drugs prescribed in a PrEP regimen — short for pre-exposure prophylaxis — block the virus that causes AIDS from multiplying in a person’s body. They can be taken in either pill or injection form on an ongoing basis. PEP refers to post-exposure prophylaxis and involves taking medication within 72 hours of potential exposure and for a short period of time, in order to prevent infection and transmission of the virus. Both regimens are recommended by the Centers for Disease Control and Prevention as effective ways to reduce the spread of HIV/AIDS when used correctly.
The U.S. Preventive Services Task Force was created in 1984 by congressional authorization to issue evidence-based advice to physicians on which screenings and preventive medicines are worth considering for their healthy patients. The panel’s recommendations are closely watched by professional societies when adopting guidelines for their clinician members. In many cases, when insurers are on the fence about whether to cover a given screening or diagnostic test, they’ll turn to the panel’s recommendations.
The panel, made up of doctors, nurses, health psychologists, epidemiologists and statisticians who are experts in primary care and preventive medicine and who serve four-year terms on a voluntary basis, is meant to be free from conflicts of interest and outside influences.
Some of its past recommendations, however, such as its advice on prostate cancer screenings, have been met with criticism.
When it comes to HIV prevention, the U.S. Supreme Court appeared to back up the task force with its July 11 ruling in Kennedy vs. Braidwood Management, which upheld a key mandate in the Affordable Care Act requiring insurers to cover preventive care, including for HIV.
However, in the same ruling, the court also declared that the Secretary of Health and Human Services has the power to review decisions made by the task force, and to remove members at his or her discretion.
Kennedy abruptly postponed the task force’s July meeting, sparking concern among public health advocates and Democratic leaders.
“The task force has done very little over the past five years,” Kennedy said at Monday’s news conference. “We want to make sure that it is performing, that it is approving interventions that are actually going to prevent the health decline of the American public.”
González said he worries that the Supreme Court gave the administration a new way to meddle in the healthcare decisions of LGBTQ+ people.
“The Braidwood decision was both a relief and a wake-up call,” González said. “While it upheld the Preventive Services Task Force’s existing recommendations — keeping protections for PrEP, cancer screenings, and vaccines intact — it handed unprecedented authority to RFK Jr. to reshape that very task force and place existing protections under direct threat once again.”
González described AB 554 as “a measure to protect LGBTQ+ Californians and ensure we never return to the neglect and devastation of the HIV/AIDS crisis.” The state Senate Appropriations Committee is expected to vote on whether to advance the bill on Aug. 29.
“These attacks aren’t isolated,” the lawmaker said. “They are coordinated, deliberate, and aimed squarely at our most vulnerable communities.”